Does Blue Cross Fep Cover Covid Antibody Test
In accordance with the Families First Coronavirus Response Act CareFirst is covering the antibody test for SARs-CoV-2. Yes Blue Cross Blue Shield members will not have to pay for COVID-19 diagnostic tests that are performed by a licensed or authorized health care provider through October 18 2021.
Thats a big step toward stopping the spread of the virus.
Does blue cross fep cover covid antibody test. The FDA has approved several vaccines for emergency use authorization. All Anthem plans will cover medically necessary screening and testing for COVID-19 and will waive all cost shares co-pays coinsurance and deductibles. You can still get an antibody test if youve had the COVID-19 vaccine.
No prior authorizations for diagnostic tests and covered services FEP will waive prior authorizations for diagnostic tests and for covered services that are medically necessary and consistent with CDC guidance if diagnosed with COVID-19. More than 140 million Americans have received a dose of the COVID-19 vaccine. No Blue Cross doesnt cover the cost of workplace or occupational screening tests for COVID-19.
CareFirst and plan sponsors will cover the full cost of in-network deductibles copays and coinsurance for FDA-authorized and medically necessary antibody testing when ordered by a doctor nurse practitioner or other authorized provider. Blue Cross and Blue Shield of Illinois BCBSIL is closely monitoring activity around the Novel Coronavirus 2019 COVID-19. To be covered by CareFirst the test should.
See below for those not covered This means you do not need to pay out-of-pocket costs copay coinsurance or deductible for tests that are provided or ordered by a healthcare provider. No early medication refill limits. The COVID-19 test is 0 for all members and through Aug.
Information about serological test performance characteristics are displayed in this Independent Evaluation of SARS-CoV-2 Antibody Test Performance. Be ordered by a physician or other authorized provider. No cost share for COVID-19 vaccines.
Weve taken steps to lower costs and provide our members easier access to care related to COVID-19. With a BCBSIL health plan you have access to care for COVID-19 related health issues. This includes screenings andor tests that take place at in-person office visits drive-through sites virtual on-line visits and telephone calls.
Yes antibody tests for COVID-19 testing are covered at 100 with no member cost sharing as required by the Families First ActCARES Act. It does not include testing for people without symptoms and no suspected exposure. Find a COVID-19 testing location near you by using this tool.
Part B covers certain doctors services outpatient care medical supplies and preventive services. Tests with FDA Emergency Use Authorization have varying degrees of accuracy. Testing and Treatment Coverage.
That is why our Florida Blue Center teams are here to provide support for you and your patients. Blue Shield and Blue Shield Promise cover most diagnostic tests for individuals at no out-of-pocket cost to you. Labcorp will bill the cost of the COVID-19 antibody test directly to your health plan if you are insured or if you are uninsured Labcorp will bill the appropriate government program.
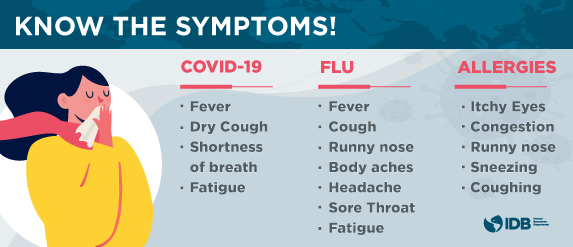
However antibody testing does NOT indicate if an individual has an active COVID-19 infection. No cost share for diagnostic tests or treatment. Be on the EUA list.
Covers a COVID-19 antibody or serology test. An antibody test does not detect the presence of the SARS-CoV-2 virus to diagnose COVID-19. If you charge the member a cost share at the time of service you may need to reimburse the member when you receive your voucher.
No prior authorizations for diagnostic tests and covered services. But some are still hesitant to get the shot. Exclusions to this coverage include testing for the following.
However we do cover the cost of testing if a health care provider orders an FDA-approved test and determines that the test is medically necessary. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. 31 were waiving the cost share for covered services for the treatment of those with a positive COVID-19 diagnosis.
The cost of the test is 4213 and is based on rates established by the Centers for Medicare Medicaid Services CMS. Thats why during this time FEP is making some benefit changes to ensure you have access to the right care at the right time. Coronavirus disease 2019 COVID-19 antibody test.
Use the doctors labs and facilities in your BCBSIL health plans provider network for. Antibody testing is not currently recommended to assess for immunity to COVID-19 following vaccination. BCBSTX is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order.
For testing performed out of network CareFirst or the plan sponsor will pay 100 up to charge. People booking a PCR test for COVID-19 will also be given the option to take part in antibody testing. We have transitioned our walk-in Florida Blue Centers to virtual support and services and our locally based nurses community specialists and service specialists are just a phone call away.
COVID-19 testing is available at no cost. Call us at 877-352-5830 with questions about COVID-19. Have a high likelihood of impacting clinical decision making.
To ensure you have access to the right care at the right time FEP is waiving cost shares and prior authorization to support members care for COVID-19. This includes testing for people who have been exposed or may have been exposed to someone with COVID-19. Are antibody tests used to diagnose COVID-19.
When are COVID-19 tests covered. A nurse case manager with Blue Cross Blue Shield of Rhode Island found that listening without judgment to one patients concerns made all the difference. Tests to diagnose COVID-19.
Lab tests to diagnose COVID-19 are covered at no cost. To be covered by your BCBSRI health plan your COVID-19 test must be medically necessary and ordered by a healthcare provider. A doctor must order a COVID-19 test for you.
Waiving cost-sharing for COVID-19 testing and treatment. Please talk to a doctor first to be certain you need a COVID-19 test. We suggest you bill Blue Cross or BCN first for COVID -19-related services and wait for the voucher remittance advice to determine member cost share liability.
All Anthem plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs. These are covered based on your benefit plan. Through May 31 all BCBS companies including the BCBS Federal Employee Program FEPare.
Your Blue Cross and Blue Shield of Illinois BCBSIL health plan gives you access to the care you need during the COVID-19 pandemic.
Coronavirus Antibody Test How It Works Accuracy Where To Get One
Covid 19 Info For Clinical Partners
Covid 19 Info For Clinical Partners
Coronavirus Updates Blue Cross Of Idaho
Information Regarding Coronavirus Covid 19 Highmark Bcbswny
Covid 19 Coronavirus Resource Center Benefit Changes Blue Cross And Blue Shield S Federal Employee Program
Your Frequently Asked Questions About Covid 19 Coronavirus
Bcbs Covid 19 Info Benefits Testing And More Blue Cross And Blue Shield S Federal Employee Program
Blue Cross Coverage Of Covid 19 Testing What To Know Mibluesperspectives
Covid 19 Coronavirus Resource Center Benefit Changes Blue Cross And Blue Shield S Federal Employee Program
Testing For Covid 19 Faqs Blue Shield Of Ca
Bcbs Covid 19 Info Benefits Testing And More Blue Cross And Blue Shield S Federal Employee Program
Bluecross Blueshield Of South Carolina And Bluechoice Healthplan Of South Carolina Inc Group Eligibility Guidelines Related To Covid 19 Pandemic Bluechoice Healthplan Of South Carolina
Coronavirus Your Health Care Premera Blue Cross
Service Horizon Blue Cross Blue Shield Of New Jersey


Posting Komentar untuk "Does Blue Cross Fep Cover Covid Antibody Test"