Is Rapid Covid Test Covered By Insurance Aetna
Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. Aetna is here for you during the coronavirus COVID-19 pandemic no matter what.

Coronavirus Covid 19 Resources Aetna Medicaid Illinois
Stay home and isolate.
Is rapid covid test covered by insurance aetna. A test must be covered if your attending health care provider has assessed your individual situation and determined that it is medically appropriate you have symptoms or have a known or likely recent exposure to COVID-19. Medicaid patients may not pay out of pocket for Rapid COVID Testing. Learn about extra benefits and well-being resources just for you find testing locations get answers to the most frequently asked questions regarding COVID-19 and tips to stay safe and much more.
Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services. Insurers are legally required to pay for in-network testing so try to find a medical facility where you know youll be covered. For Medicare CMS has indicated it will cover the full cost of the vaccine for all Medicare beneficiaries including those in.
And second youre in luck. CVS Health has been increasing access to testing options since the start of the pandemic and has completed more than 15 million COVID-19 tests to date across more than 4800 testing sites at select CVS Pharmacy locations with nearly 1000 of those locations providing rapid. Tests to diagnose or aid the diagnosis of COVID-19.
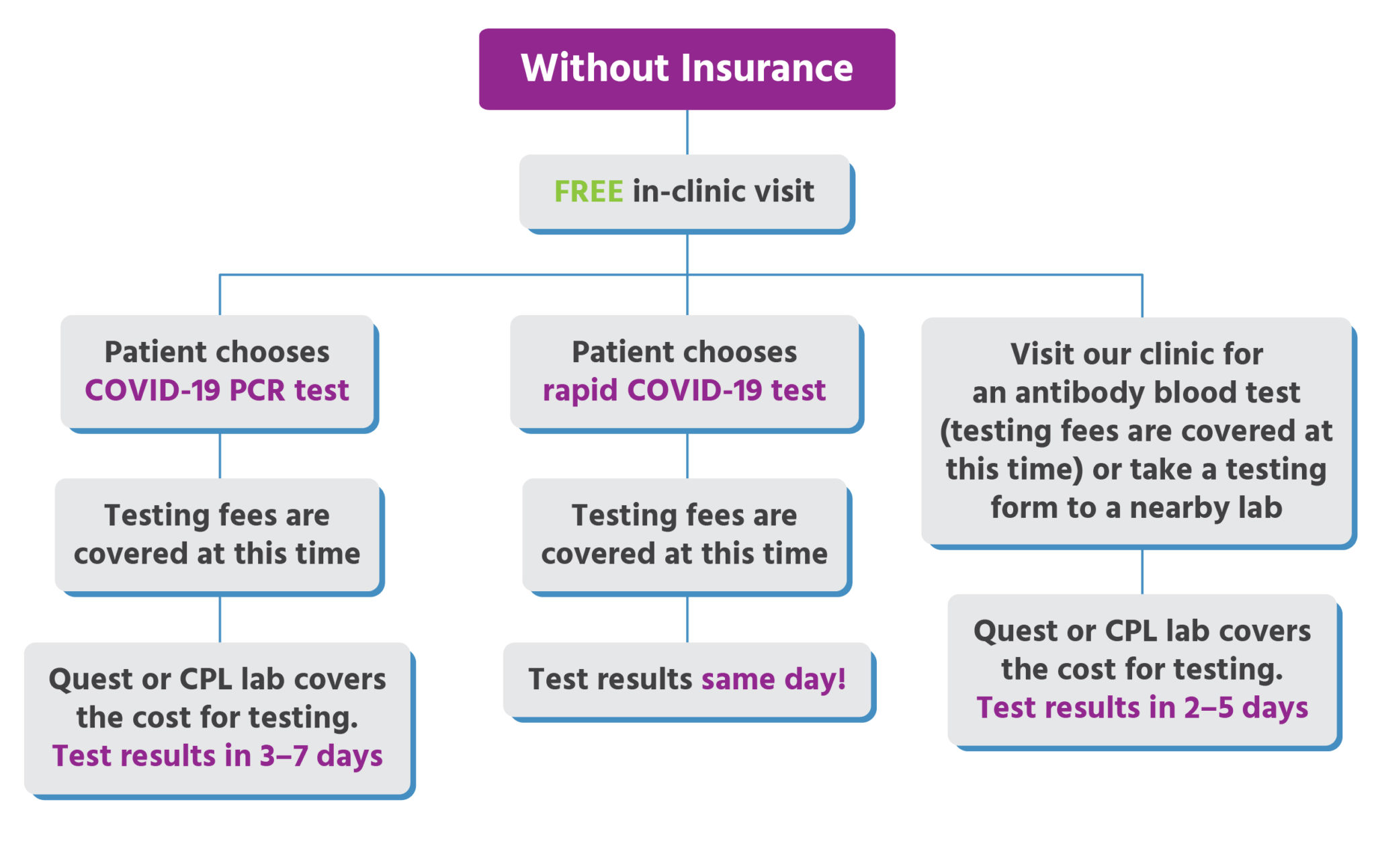
Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test. The OTC testing options are not covered by insurance and are not meant to test the efficacy of COVID-19 vaccination. Insurance Non-Covered for Rapid COVID Test Medicaid Keystone First Health Partners Aetna Better Health UHC Community Plan Generally Rapid COVID-19 testing is not covered but standard NAA testing is usually covered.
Extremely Urgent RT-PCR COVID-19 Test result in 1 hour. Visit our COVID-19 FAQ page for answers to the most frequently asked questions regarding the coronavirus and to get the latest information. A completes the test in two calendar days or less and b completes the majority of their COVID-19 diagnostic tests that use high throughput technology in two calendar days or less for all of.
CVS Health also currently offers COVID-19 diagnostic testing using molecular- or antigen-based tests to identify an active infection at more than 4800 CVS Pharmacy locations nearly 1000 of which provide rapid-result testing. Members Aetna is here to keep you informed during the coronavirus COVID-19 pandemic. What should I do if I test positive for the virus.
The test can be done by any authorized testing facility. And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test will only be a covered. According to its website as of Nov.
If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. This member cost-sharing waiver applies to all Commercial Medicare and Medicaid lines of business. Rapid Antigen Test results in 10 minutes.
Rapid COVID-19 Antigen Test with Insurance. The answer is up for interpretation. As announced by CMS starting January 1 2021 Medicare will make an additional 25 add-on payment to laboratories for a COVID-19 diagnostic test run on high throughput technology if the laboratory.
To date the company has administered more than 15 million COVID-19 diagnostic tests. Rapid tests like the ones offered at the airport on the day of travel might not be covered by many insurance companies. This member cost-sharing waiver applies to all Commercial Medicare and Medicaid lines of business.
In addition Aetna is waiving member cost-sharing for diagnostic testing related to COVID-19. Insurers will be making judgment calls likely on a case-by-case basis about how they will handle cost sharing for screening. 9 2020 Aetna is waiving member cost-sharing for diagnostic testing related to COVID-19 done by any authorized testing facility.
The test can be done by any authorized testing facility. When tests are available for you in your state Medicare covers and you pay nothing for. Covers a COVID-19 antibody or serology test.
In addition Aetna is waiving member cost-sharing for diagnostic testing related to COVID-19. Generally only PCR Test is covered under these health insurance. State variations and regulations may apply.
If you have health care coverage directly from an insurance company the health insurance marketplace or through your employer including through COBRA. You do not need to obtain a referral from a physician in order to get a COVID-19 test and have it covered by Medicare. Coronavirus disease 2019 COVID-19 antibody test.
Many insurers have also agreed to cover the cost of a COVID test if its done at an out-of-network facility but youll want to reach out to your insurance company or MedicareMedicaid provider before your visit. Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings. Aetna a CVS Health company is waiving member cost-sharing related to the COVID-19 vaccination for Commercial and Medicaid members.
Medicaid Keystone First Health Partners Aetna Better Health UHC Community Plan Generally Rapid COVID-19 testing is not covered but standard PCR testing is usually covered. Is your COVID test covered. Aetna Cigna Healthfirst MetroPlus MVP United Health Care Oxford Members ONLY.
Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you. Tests to detect antibodies to the virus must be covered free of charge under health insurance plans and Medicaid according to new guidance issued by the federal government.
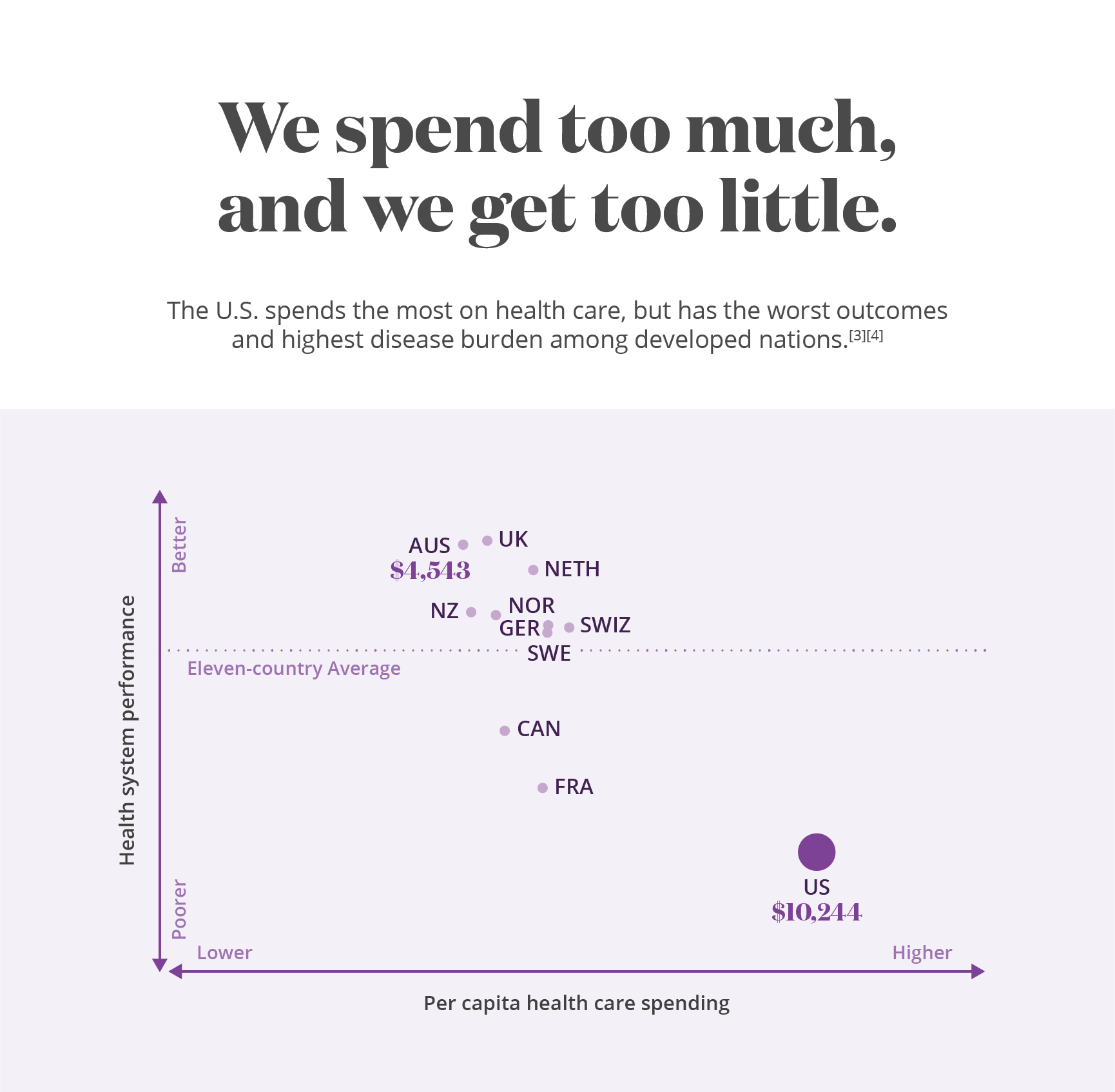
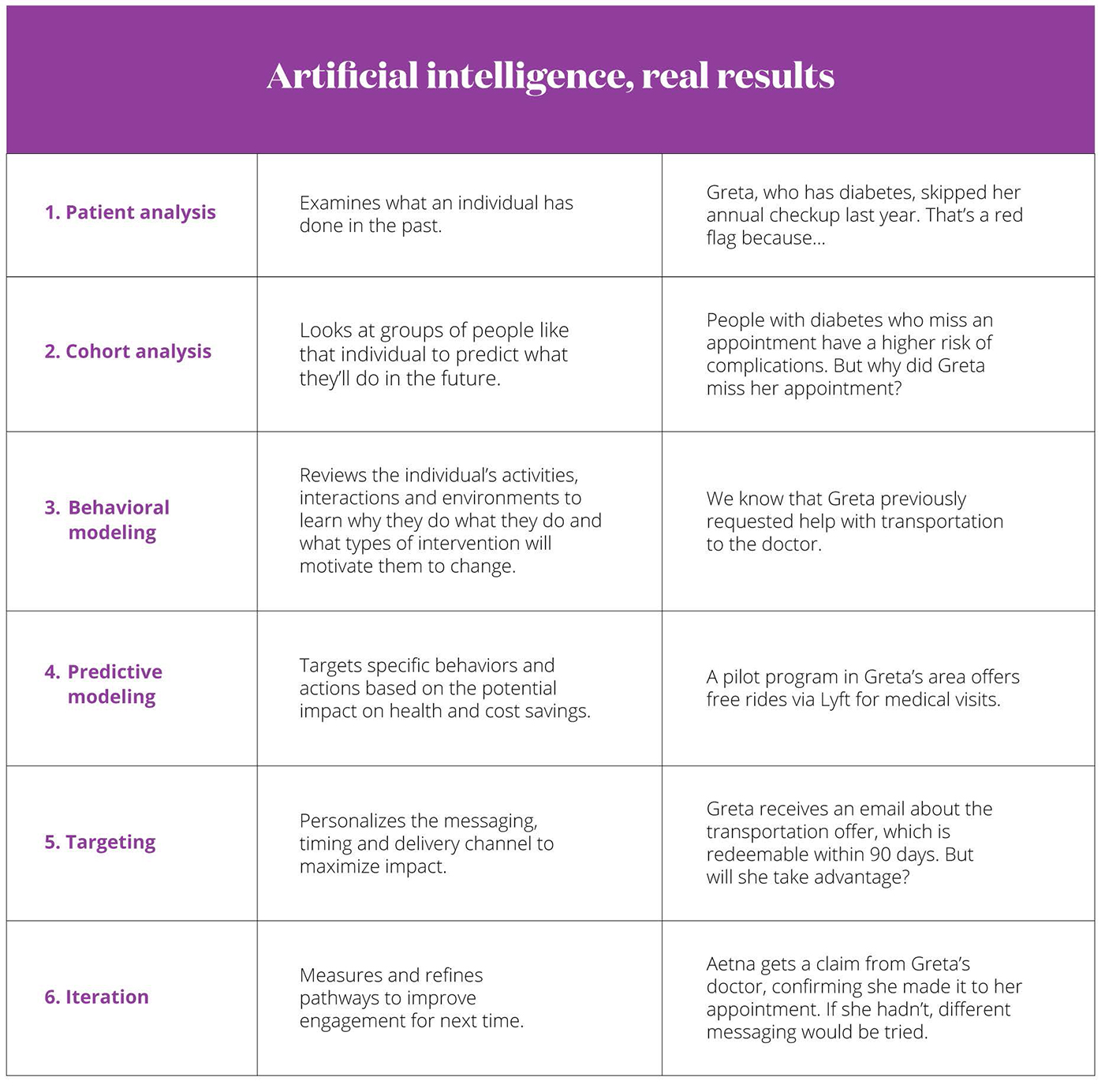
What Is Value Based Care How It Works Benefits I Aetna

Cvs Health Announces Availability Of Covid 19 Antibody Testing At Minuteclinic Locations Across The Country Cvs Health
What S In A Covid 19 Test Northwell Health

Covid 19 Testing Bills Surprise New Yorkers Modern Healthcare

Westminster Urgent Care Covid 19 Testing Results In An Hour
Urgent Care For Kids Insurance Accepted Cost

How To Stop Paying For Expensive Covid Testing News Wsmv Com
Health Care Plan Benefits Human Resources Vanderbilt University

Covid 19 Resources Support For Aetna Providers

Adventhealth Centra Care Doubles Covid 19 Rapid Testing Services Offers Expanded Services And Hours
Aetna Waives Co Pays For Covid 19 Screenings News Vanderbilt University

Administrators Aetna Student Health
Que Es La Precision Medicina Y Como Puede Ayudar Aetna

Know Where To Go For Care Texas Health Aetna

More Sites To Conduct Covid 19 Rapid Tests Northwell Health
Posting Komentar untuk "Is Rapid Covid Test Covered By Insurance Aetna"