Health Coverage Transparency Rules
The rule does not apply to Medicare Medicaid grandfathered health plans standalone vision or dental plans short-term limited duration plans HRAs FSAs or HSAs. The Transparency in Coverage final rule released today by the Department of Health and Human Services HHS the Department of Labor and the Department of the Treasury the Departments delivers on President Trumps executive order on Improving Price and Quality Transparency in American Healthcare to Put Patients First.

President Trump S Record On Health Care Kff
This rule which was included in last Decembers omnibus spending bill is aimed at protecting patients from unexpected out-of-network bills.

Health coverage transparency rules. In October 2020 CMS released the TiC Final Rules which require group health plans and health insurance carriers carriers to publicly post standard charge information and negotiated rates for common shoppable items and services in an easy-to-understand consumer-friendly and machine-readable format. Final transparency-in-coverage rules require group health plans and insurance issuers in the individual and group markets to disclose extensive price and cost-sharing information beginning in 2022. On October 29 2020 HHS and the Departments of Labor and Treasury finalized a Transparency in Coverage Final Rule requiring most health plans and issuers in the individual and group commercial markets to disclose cost-sharing estimates and additional content to enrollees upon request and to publicly post negotiated in-network provider rates historical out-of-network allowed amounts and.
Just before Halloween the Departments of Treasury Labor and Health and Human Services the Departments released their final rule on health plan price transparency. Current Status of Final Rule 4 If Supreme Court Decision Texas v. In October 2020 the Departments released final rules on the transparency in coverage requirements that apply to group health plans they.
Doesnt the rule violate HIPAA or other security or privacy rules. In simple terms it means employer-sponsored group health plans and health insurance issuers in the individual and group markets are going to be required to make cost-sharing information available upon request to members. Within the last year Congress and the Departments of Treasury Labor and Health and Human Services the Departments have issued a bevy of new rules for group health plans that aim to encourage transparency in health care costs and compliance.
HUBs EB Compliance Team. No Surprises Act health plan transparency requirements of the Consolidated Appropriations Act 2021 CAA and the Health Coverage Transparency Final Rule Multiemployer Plan Considerations General Considerations The NCCMP supports the objectives of the No Surprises Act to protect plan participants from surprise medical bills. Transparency in Coverage Final Rules.
Both the final regulation on Transparency in Coverage TiC rule issued October 29 2020 and the transparency requirements provisions for plans and issuers within the Consolidated Appropriations Act of 2021 CAA require notice and disclosure of health plan costs beginning either December 27 2021 or January 1 2022. 1 See Departments finalize transparency in health coverage rule Insider November 2020. The forthcoming laws complement the Hospital Price Transparency Rule in making it easier for patients to compare care costs avoid surprise bills and know the price of care in advance.
The requirements phase in over three years with the first compliance requirements becoming effective January 1 2022 and they present a dramatic expansion of price transparency for health. 1 This final rule is a historic step toward putting health care price. On December 6 2020 we posted an article titled RADICAL new transparency rules likely apply to your health plan in one year.
Chamber of Commerce and the Pharmaceutical Care. 2 The term grandfathered is defined in section 1251e of the Affordable Care Act and is used by the IRS DOL Centers for Medicare Medicaid Services and HHS to refer to certain group health plans and health insurance coverage existing as of March 23 2010 the enactment date of the. In case you havent heard the IRS Department of Labor and Department of Health and Human Services have issued the Transparency in Coverage ruleBut what exactly is it.
While the Transparency in Coverage Rule applies directly to group health plans an issuer or third-party administrator TPA may support the compliance requirements for the group health plan. On November 15th the Department of Health and Human Services the Department of Labor and the Department of the Treasury collectively the Departments released the Transparency in Coverage proposed rules outlining a new set of healthcare pricing transparency requirements targeted at giving patients access to pricing information directly through their health plans. California renders ACA unconstitutional transparency rule will become ineffective expected decision in 2021 session Potential future litigation challenges.
Two New Lawsuits Challenge Insurer Transparency Rule. This rule entitled Transparency in Coverage requires group health insurance carriers and self-insured plans to disclose rates and cost-sharing information for all covered items and services. Hot off the Press.
In addition to the Transparency in Coverage Rule health plans will need to comply with the No Surprises Act which also goes into effect next January. Health Coverage Transparency Rules. On Friday 820 the Department of Labor issued an update around the timeframe and enforcement of both Transparency in Coverage and the No Surprises Act for payer price transparency.
As part of this project CMS has also added a shared-savings provision to the medical loss ratio MLR rules. On January 1 2022 parts of the new federal transparency rules Transparency in Coverage and the No Surprises Act will go into effect mandating employer plan sponsors and health plans to. Within two days the US.
More details on transparency rules that apply in 2022 and beyond. The rules also include proposals to require plans and insurers to disclose in-network provider negotiated rates and historical out-of-network allowed amounts through an internet website thereby allowing the public to have access to health insurance coverage information that can be used to understand healthcare pricing and potentially dampen the rise in healthcare spending.

Data Management Vs Data Governance Data Science Learning Strategy Infographic Data Science

Drone Infographics Buy Or Renew Car Insurance Policies Online Buy Car Insurance Policy In Easy Ste Car Insurance Renew Car Insurance Car Insurance Online
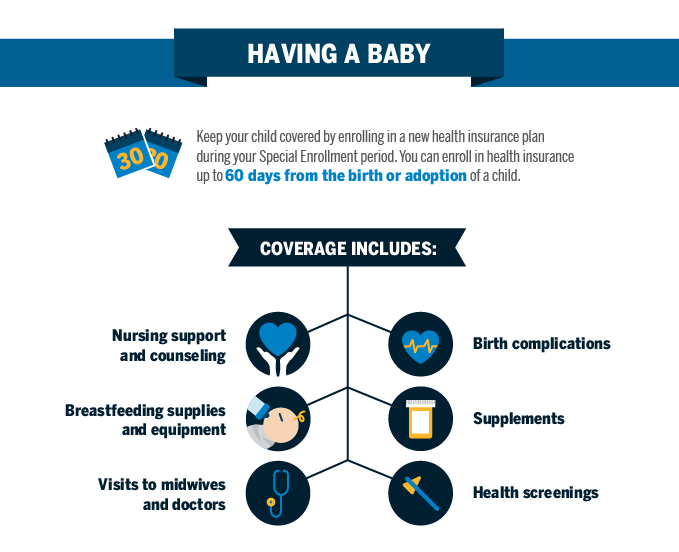
Qualifying Event Baby Blue Cross And Blue Shield Of Texas

The Future Of U S Health Care Replace Or Revise The Affordable Care Act Rand

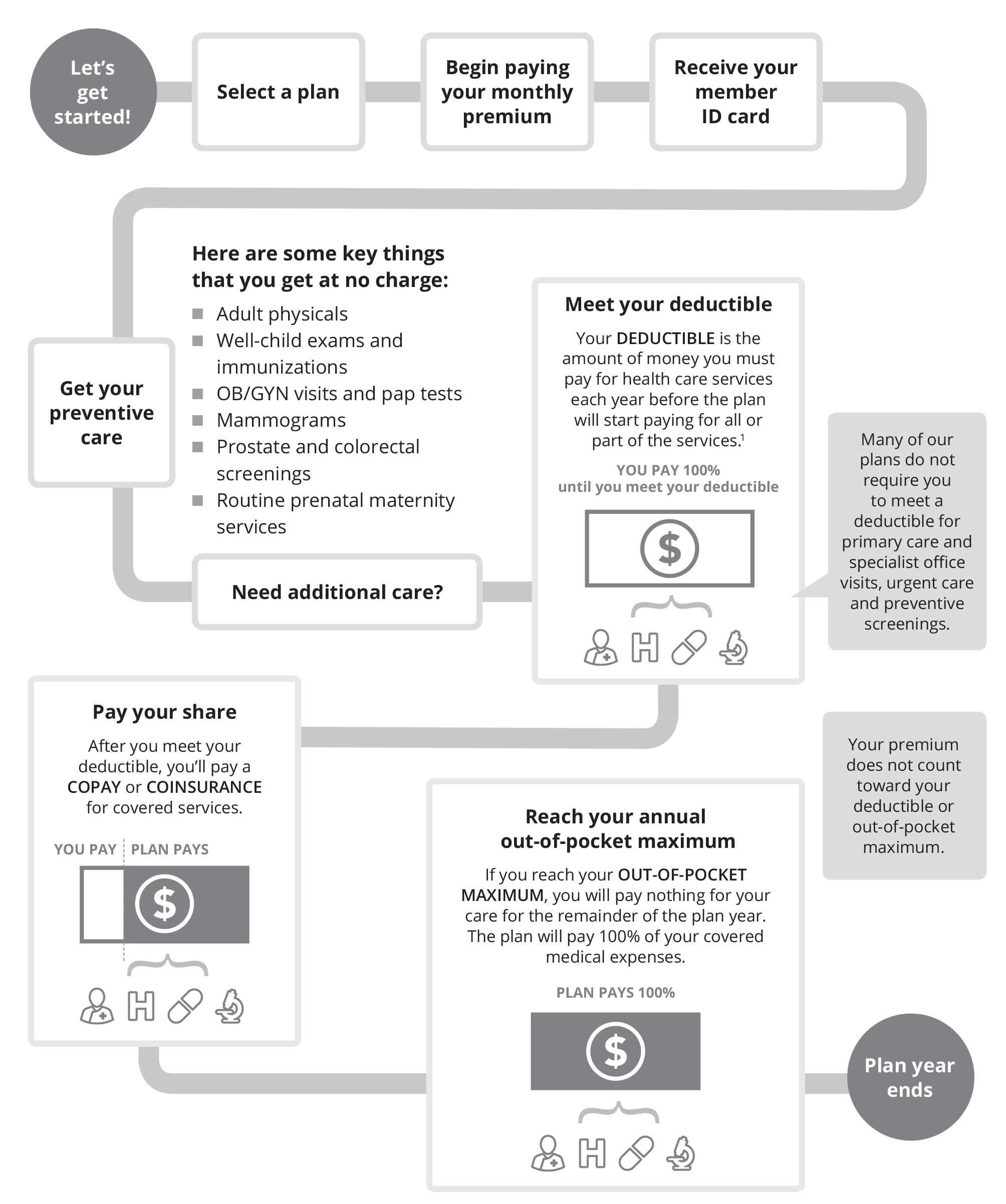
Cost Sharing Health Insurance 101 Blue Cross Nc

Barriers To Price And Quality Transparency In Health Care Markets Rand

Will Health Consumers Morph Into Health Citizens Healthconsuming Explains Part 5 Health Care Policy Health Care Coverage American Medical Association

Paying Insurance Bills Health Insurance 101 Blue Cross Nc

Functions Of Irda Compare Insurance Commercial Vehicle Insurance Business Insurance
Health Insurance Costs Carefirst Bluecross Blueshield

Cost Sharing Health Insurance 101 Blue Cross Nc
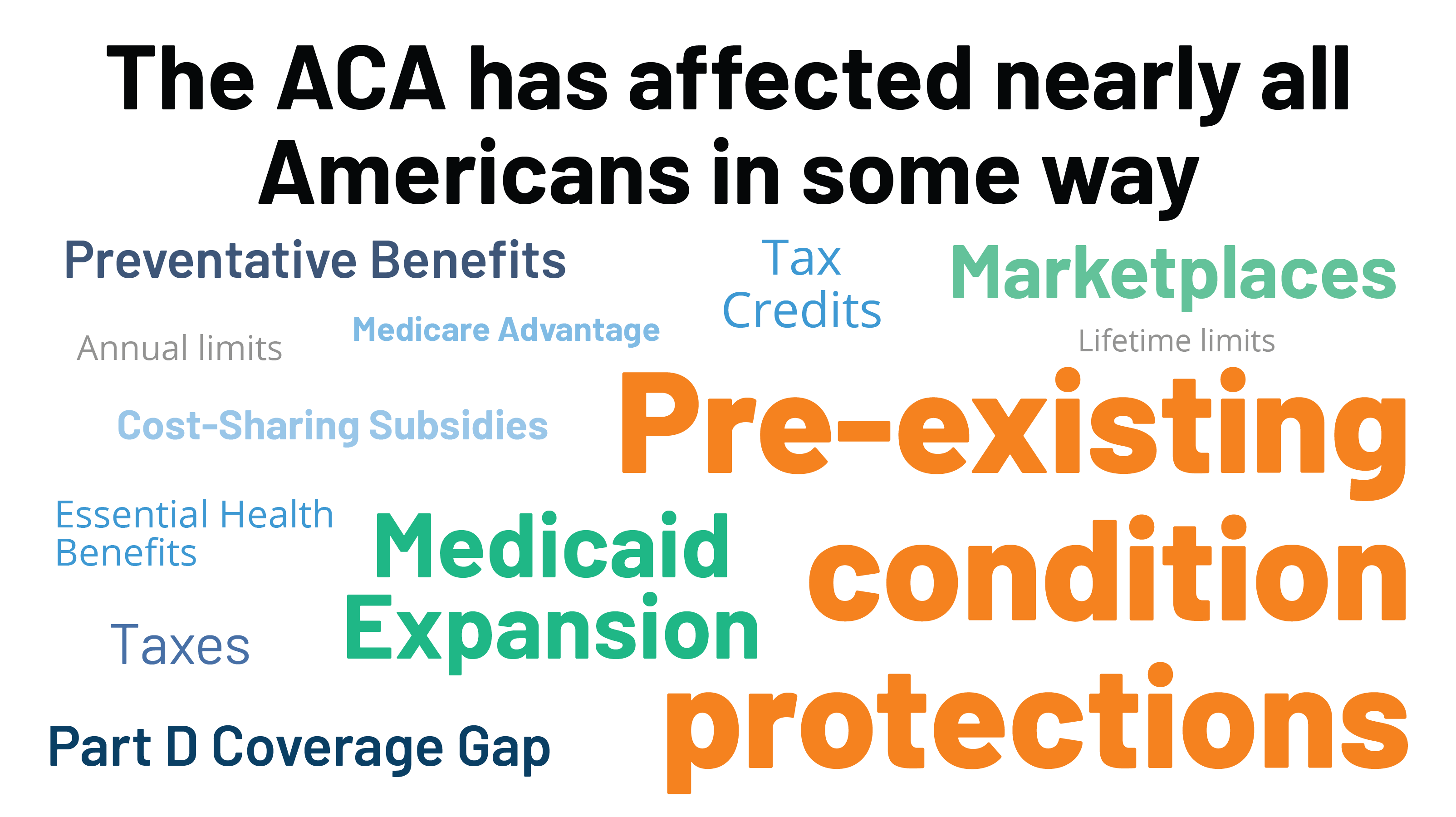
Potential Impact Of California V Texas Decision On Key Provisions Of The Affordable Care Act Kff
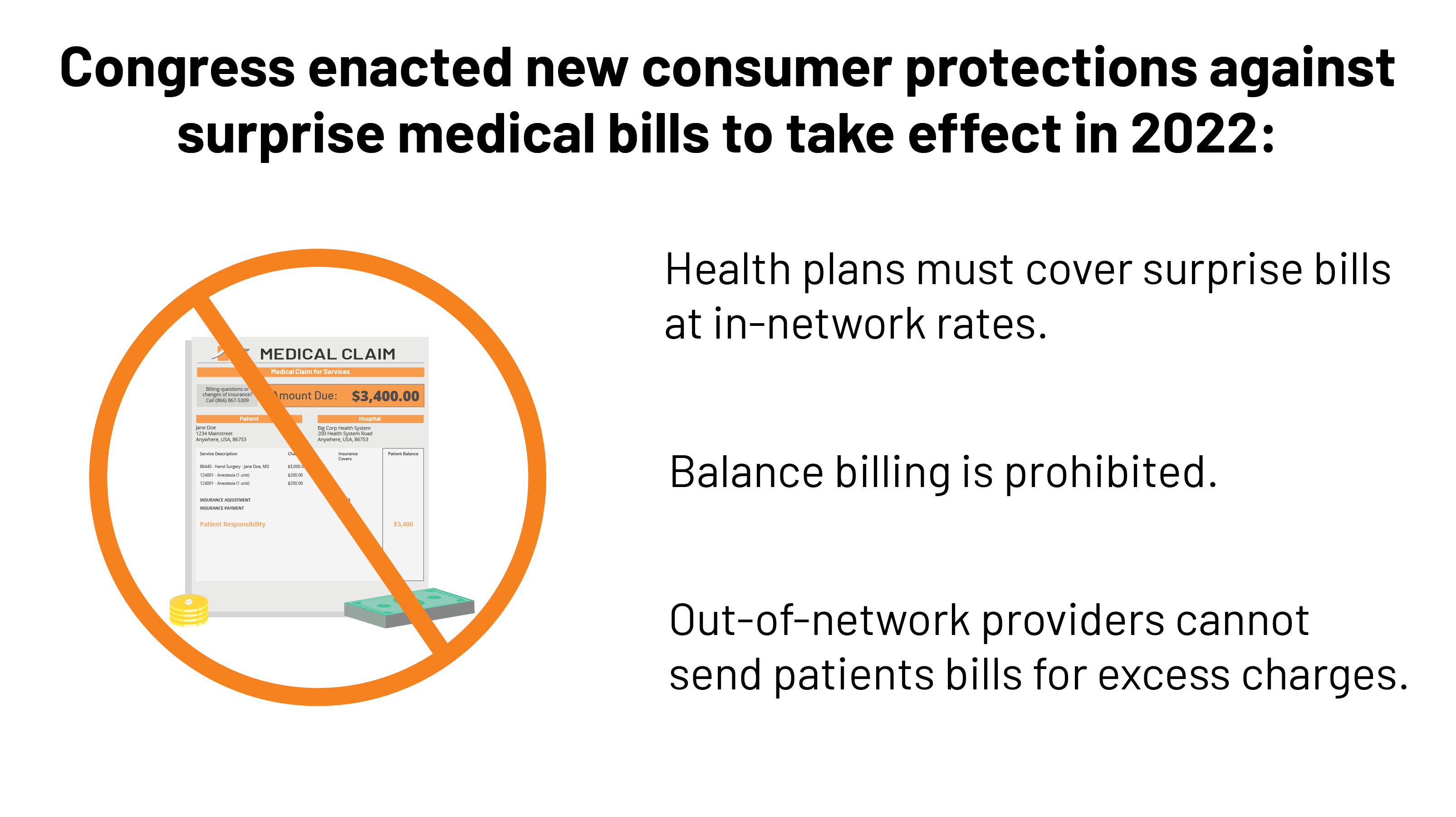
Surprise Medical Bills New Protections For Consumers Take Effect In 2022 Kff

The Future Of U S Health Care Replace Or Revise The Affordable Care Act Rand

Health Insurance Powerpoint Slides


Posting Komentar untuk "Health Coverage Transparency Rules"